9:07 AM 1/31/2022 - If the test for the specific pathogen: Sars-Cov-2 was introduced only in December of 2019, how do you know if it was not Endemic (vs. causing the Pandemic) before that time?
- Get link
- X
- Other Apps
#CIA #DOD #FBI #ODNI #NSC #POTUS #Covid19 https://t.co/weSNk1Fc6o
— Michael Novakhov (@mikenov) January 31, 2022
9:07 AM 1/31/2022
If the test for the specific pathogen: Sars-Cov-2 was introduced only in December of 2019, how do you know if it was not Endemic (vs. causing the Pandemic) before that time? Simply, there was not the test to detect and diagnose it. Therefore the historical Covid-19 may be mostly the statistical phenomenon, and possibly the weapon of the Information Warfare.
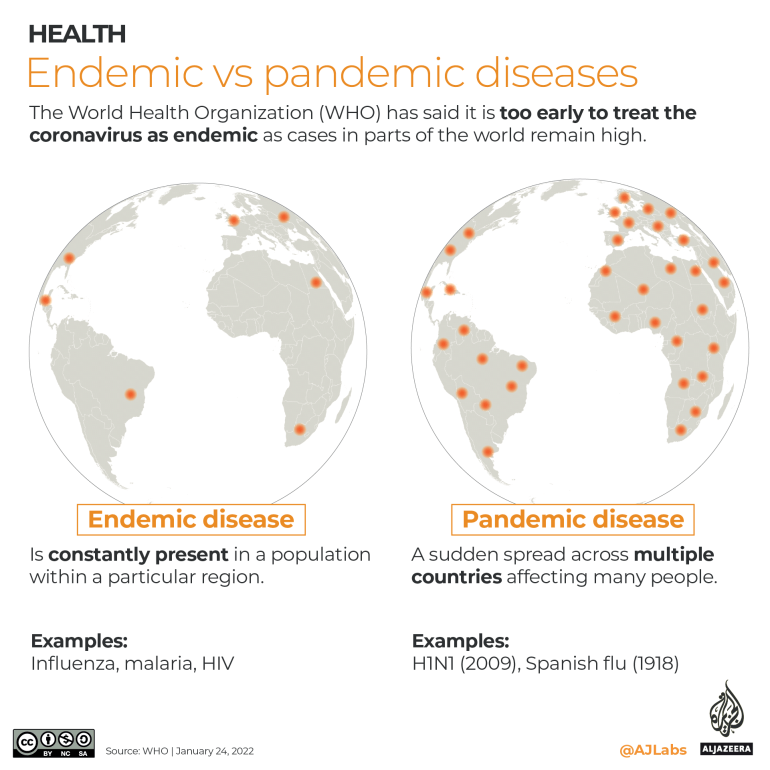
The WHO has said calls to treat the coronavirus as endemic are premature as cases in parts of the world remain high.
On March 11, 2020, the World Health Organization declared COVID-19 a pandemic – a new disease that has spread around the world, affecting a large number of people.
The term pandemic comes from the Greek word “pan” meaning “all” and “demos” meaning “people”.
In comparison, an endemic – with the prefix en- meaning “in or within”- is the constant presence of a disease within a region, making its spread more predictable.
Many experts expect COVID-19 will not be eradicated, and the disease will become endemic and stay with us, in a milder form.
While the conditions to reclassify COVID-19 as endemic are not precisely defined, many countries – particularly in Europe – have begun lifting restrictions as they move towards living with the disease.
Last week, Spanish Prime Minister Pedro Sanchez called on European officials to treat COVID-19 as endemic due to falling death rates.
Classifying COVID-19 as such could mean that fewer resources would be allocated to combat the disease and people would be subject to less testing as it would likely no longer be considered a severe public health emergency.
But the World Health Organization (WHO) has said it is too early to treat the coronavirus as endemic as cases in parts of the world remain high.
Comparing endemic diseases
Endemic diseases are all around us, from the common cold to more severe diseases including HIV, malaria and tuberculosis.
Epidemiologists, scientists who study the spread of diseases, consider a disease endemic when its levels are consistent and predictable. Endemic diseases are constantly present in a population within a particular region.
Below we compare the number of cases and deaths per year from endemic diseases.
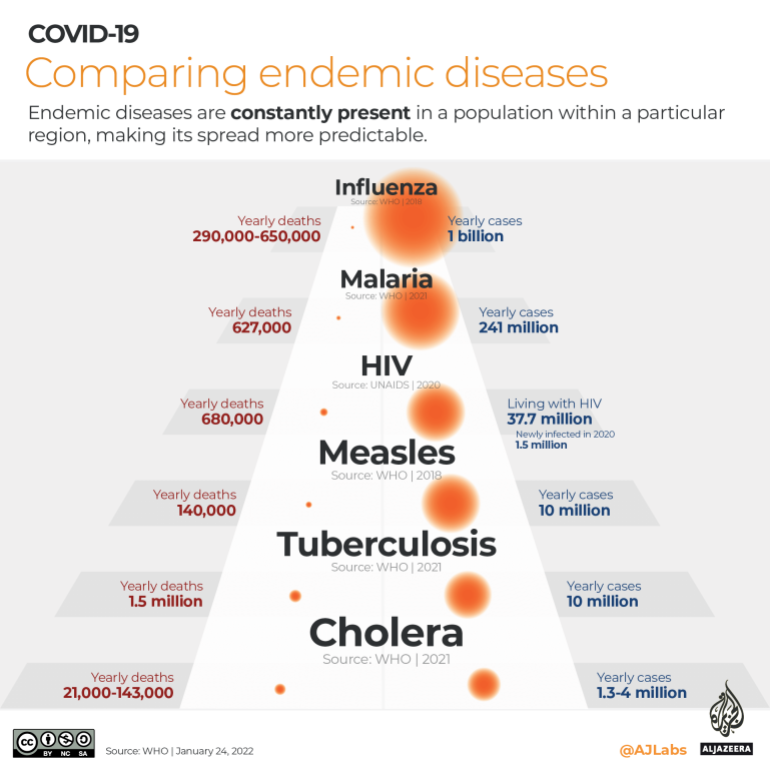
For COVID-19 to become endemic, several factors would need to be considered, including how the disease continues to evolve as well as the type of immunity people acquire through infection and vaccines.
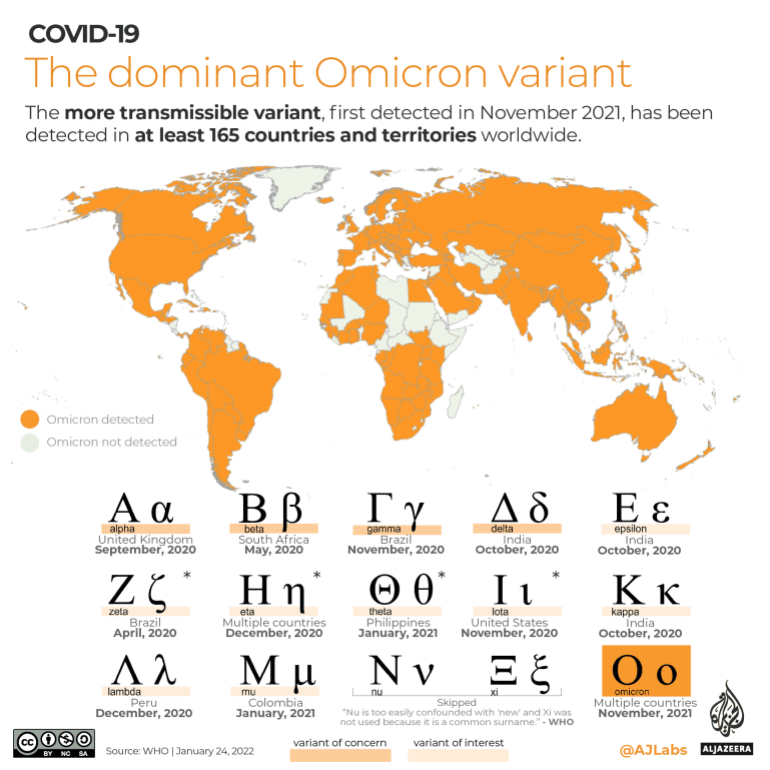
The dominant Omicron variant
Like all viruses, the SARS-COV-2 coronavirus has been mutating since it emerged in late 2019.
Mutations – changes in genetic code – in a virus’s spike protein can affect its ability to infect cells.
Omicron, a more transmissible variant first detected in November 2021, has now been detected in at least 165 countries and territories worldwide.
It has pushed COVID-19 cases to record highs around the world with at least 100 countries recording their all-time highest daily confirmed cases since the start of 2022. There are also an unknown number of people who may have been infected with Omicron but were not tested.
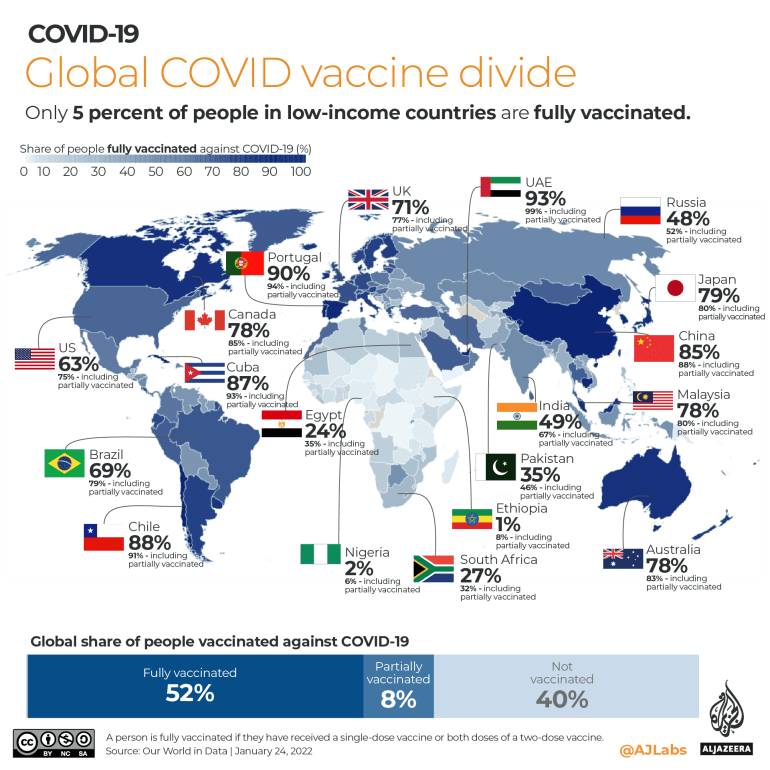
Varying worldwide immunity levels
The WHO predicts more than half of the people in Europe could catch Omicron by March which, coupled with high vaccine rates, should lead to higher levels of immunity.
Herd immunity occurs when a large proportion of a community becomes immune to a disease through infection or vaccines, halting the disease from spreading.
As variants become more infectious, the herd immunity threshold increases. This is why the threshold percentage has gradually been increasing from about 60-70 percent during the original strain to 85 percent with Delta and upwards of 90 percent with Omicron.
Meanwhile, many poorer countries that are still waiting for vaccines may be a long way from seeing the end of the pandemic.
Only 5 percent of people in low-income countries are fully vaccinated according to the latest figures by Our World In Data.
Scientists and health officials around the world are keeping their eyes on a descendant of the omicron variant that has been found in more than 50 countries, including the United States.
This version of the coronavirus, which scientists call BA.2, is widely considered stealthier than the original version of omicron because particular genetic traits make it somewhat harder to detect. Danish scientists reported this week that preliminary information suggests it may be 1 1/2 times more contagious then the original variant.
But scientists say there’s a lot they still don’t know about it, including whether it causes more severe disease.
WHERE HAS IT SPREAD?
More than 18,000 genetic sequences of BA.2 have been uploaded to GISAID, a global platform for sharing coronavirus data, according to data collected by Scripps Research labs. The strain has been detected in at least 54 countries and 24 U.S. states.
“Thus far, we haven’t seen it start to gain ground” in the U.S., said Dr. Wesley Long, a pathologist at Houston Methodist in Texas, which identified three cases as of earlier this week.
The mutant appears much more common in Asia and Europe. In Denmark, it has spread quickly and become the dominant variant, according to State Serum Institute, which falls under the Danish Ministry of Health.
“Preliminary calculations indicate that BA.2 is one and a half times more contagious than BA.1,” the original omicron, the institute’s Dr. Tyra Grove Krause said in a press release earlier this week. If it is more contagious, “it may mean that the wave of infections will be higher and will extend further into February compared to the previous projections.”
WHAT’S KNOWN ABOUT THIS VERSION OF THE VIRUS?
BA.2 has lots of mutations. About 20 of them in the spike protein that studs the outside of the virus are shared with the original omicron. But it also has additional genetic changes not seen in the initial version.
It’s unclear how significant those mutations are, especially in a population that has encountered the original omicron, said Dr. Jeremy Luban, a virologist at the University of Massachusetts Medical School.
For now, the original omicron BA.1 and its descendant BA.2 are considered subsets of omicron. But global health leaders could give it its own Greek letter name if it is deemed a globally significant “variant of concern.”
Scientists at the UK Health Security Agency found that vaccine effectiveness against symptomatic disease appears similar for BA.1 and BA.2. Looking at all vaccine brands combined, scientists found they were about 70% effective against symptomatic disease from BA.2 two or more weeks after a booster shot.
An initial analysis by scientists in Denmark shows no differences in hospitalizations for BA.2 compared with the original omicron. They are also looking into how well current vaccines work against it. It’s also unclear how well treatments will work against it.
Doctors also don’t yet know for sure if someone who’s already had COVID-19 caused by omicron can be sickened again by BA.2. But they’re hopeful, especially that a prior omicron infection might lessen the severity if that happens.
The two versions of omicron have enough in common that it’s possible that infection with the original mutant “will give you cross-protection against BA.2,” said Dr. Daniel Kuritzkes, an infectious diseases expert at Brigham and Women’s Hospital in Boston.
Scientists will be conducting tests to see if antibodies from an infection with the original omicron “are able to neutralize BA.2 in the laboratory and then extrapolate from there,” he said.
HOW CONCERNED ARE HEALTH AGENCIES?
The World Health Organization classifies omicron overall as a variant of concern, its most serious designation of a coronavirus mutant, but it doesn’t single out BA.2 with a designation of its own. Given its rise in some countries, however, the agency says investigations into its characteristics “should be prioritized.”
The UK agency, meanwhile, has designated BA.2 a “variant under investigation,” citing the rising numbers found in the U.K. and internationally.
WHY IS IT HARDER TO DETECT?
The original version of omicron had specific genetic features that allowed health officials to rapidly differentiate it from delta using a certain PCR lab test because of what’s known as “S gene target failure.”
BA.2 doesn’t have this same genetic quirk. So on the test, Long said, it looks like delta.
“It’s not that the test doesn’t detect it; it’s just that it doesn’t look like omicron,” he said.
WHAT SHOULD YOU DO TO PROTECT YOURSELF?
Doctors advise the same precautions they have all along: Get vaccinated and follow public health guidance about wearing masks, avoiding crowds and staying home when you’re sick.
“The vaccines are still providing good defense against severe disease, hospitalization and death,” Long said.
The latest version is another reminder that the pandemic hasn’t ended.
“We all wish that it was over,” Long said, ”but until we get the world vaccinated, we’re going to be at risk of having new variants emerge.”
___
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Department of Science Education. The AP is solely responsible for all content.
— Michael Novakhov (@mikenov) January 31, 2022
- Get link
- X
- Other Apps


Comments
Post a Comment